Advertisment
The new age of phage therapy: tackling antimicrobial resistant infections
ASHP Midyear Clinical Meeting – Highlights
Antimicrobial resistance (AMR) caused an estimated five million deaths in 2019 and by 2050 this is likely to rise to 10 million as an inevitable consequence of repeated exposure to antimicrobials. This has prompted renewed interest in the use of bacteriophages – naturally-occurring viruses that infect bacteria, Dr Andrew Gainey, a paediatric infectious diseases specialist pharmacist, told the audience.
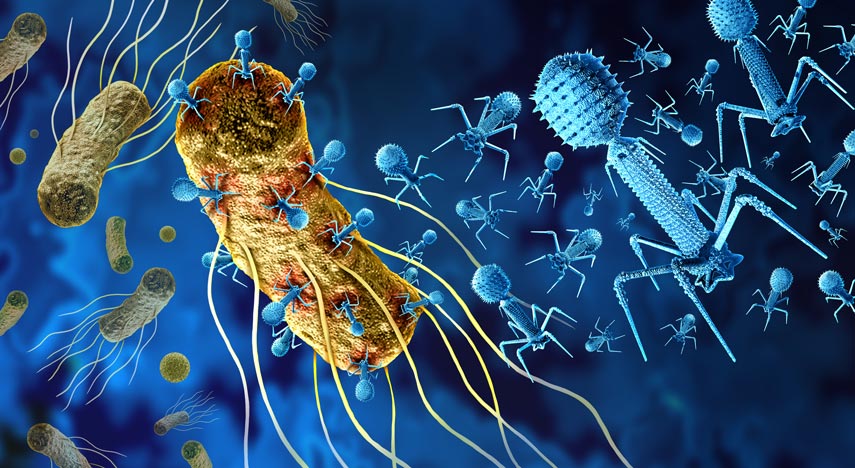
Phage therapy utilises lytic phages that attach themselves to bacteria, inject their nucleic acids, causing rapid synthesis of viral DNA and proteins so that the bacterial cells burst open releasing many more mature phages. Finding a suitable lytic phage for therapeutic use involves seeding a bacterial lawn (containing bacteria isolated from the patient) with a mixture of phages and looking for the clear areas where phages have lysed (killed) the bacteria, explained Dr Gainey. Phage banks are now being established but only limited trials have been carried out so far, he added.
By definition, bacteriophages are only suitable for bacterial infections and not for viral, fungal or parasitic infections. They are not suitable for first-line therapy, but they can be used safely in immunocompromised patients. Phages can be used singly or in ‘phage cocktails’. They can also be co-administered with antibiotics and may have synergistic actions. It has been suggested that they could resensitise an organism to antibiotics. Another useful property of phages is that they are able to penetrate biofilms. Some phages produce matrix-degrading enzymes that break down biofilms and it may be this that allows antibiotics to reach the site of action. It is possible to have phage-specific antibodies that neutralise the phages but these take time (7-10 days) to develop. Adverse effects are rarely reported.
When it comes to clinical use, phages are dosed in plaque-forming units (PFUs). It is estimated that about 10 phages are needed for each bacterial cell and that a bacterial load of at least 104 colony-forming units (CFUs) is needed for self-amplification to occur and effective treatment to start. Repeated doses are usually given and the duration of treatment is similar to that for site-specific antibiotic treatment. Thus, for example, when treating recurrent pyelonephritis, a dose of 109 PFUs, intravenously every 12 hours, may be offered. When phage treatment starts improvements can be expected after 7-10 days, said Dr Gainey. The STAMP trial (Standardised Treatment and Monitoring Protocol for Adults and Paediatric Patients) in Australia is evaluating the clinical protocol for administering and monitoring phage therapy, he added.
There are both opportunities and obstacle in the field of phage therapy at present, said Dr Gainey. Major advantages include the fact that phages are self-replicating at the site of infection, have low toxicity and are species specific. On the other hand, most evidence comes from case series rather than RCTs, time-to-treatment can be lengthy and a large bacterial burden is required “to maximise the phage burst size”, he said. Phage treatment centres are now being established and the Center for Innovative Phage Applications and Therapeutics (IPATH) at the University of California, San Diego is currently the best established.
Phage treatment successes
There have been a number of reports of successful treatments with phages and these have helped researchers to identify the most appropriate situations for phage therapy. One report concerned 16 cases of refractory Pseudomonas infections (including osteomyelitis, bacteraemia and joint infections) treated with a specific phage (PASA16). The authors reported a recovery/remission rate of 86.6 per cent.1. Ling and colleagues described how more than 30 patients with cystic fibrosis (CF) and chronic pulmonary colonisation had been successfully treated with phage cocktails.2 This had resulted in improved lung function, reductions in sputum production and coughing and, in some cases eradication of infection. A multi-centre, randomised, controlled trial of inhaled phage therapy – SWARM-P.a. – for CF was recently completed in the US. Many studies are in preliminary phases. Trials so far report minimal adverse effects associated with phage therapy.
The ideal patients for phage therapy are those with chronic colonisation or recurrent infections and those infected with drug resistant organisms. Dr Gainey described his own experiences with three patients who had received phage therapy. One was a patient with recurrent urosepsis due to infections with extended spectrum beta-lactamase (ESBL) E coli and one had CF with chronic colonisation with pan-drug resistant Achromobacter. Another patient with CF had been colonised with Mycobaterium avium complex (MAC) for six years. In each case, concurrent antibiotic treatment had been given for part of the treatment period and the phage treatment resulted in clinical improvements.
References
- Onallah H, Hazan R, Nir-Paz Ran et al. Refractory Pseudomonas aeruginosa infections treated with phage PASA16: A compassionate use case series. Med 2023: 4; 600-11 e4
- Ling K-M, Stick SM, Kicic A. Pulmonary bacteriophage and cystic fibrosis airway mucus: friends or foes? Front Med 2023: 10. https://doi.org/10.3389/fmed.2023.1088494
Dr Andrew B Gainey PharmD, AAHIVP, BCIDP, Prisma Health Children’s Hospital – Midlands; University of South Carolina College of Pharmacy. Dr Gainey gave a presentation entitled, The new age of phage therapy: Utilising viruses to treat antimicrobial resistant infections as part of the ‘Spotlight on Science’ session at the ASHP Midyear Clinical Meeting held in Anaheim, California, USA, December 3-7th 2023.






